The COVID-19 pandemic has lasted for more than two and a half years. With SARS-CoV-2’s constant mutations, neither COVID-19 vaccines nor previous infections are able to protect us completely from the newest emerging strains, as demonstrated by the recent Omicron BA.4/5 subvariants.
As a matter of fact, the primary effect of vaccination is to generate neutralizing antibodies. However, the neutralizating antibody is only a tiny part of our sophisticated natural immune system. In other words, so reduced antibody binding does not mean that we are losing our natural immunity to the mutant strains. The human body is innately capable of defending against SARS-CoV-2 and emerging viruses via natural immunity regardless of any mutations or viruses, and this article will detail how.
What Is Immunity?
Immunity is the ability of an organism to resist a particular infection or toxin.
Humans have two levels of immunity, natural and acquired. We are born with natural (innate) immunity, which protects us from all types of pathogens, instead of specific ones. Acquired (adaptive) immunity is achieved by inoculation or getting infected by specific pathogens including viruses and germs.
In a UK human challenge trial published in the journal Nature, 36 healthy volunteers aged 18 to 29 without evidence of previous COVID-19 infection or vaccination underwent 14 days of inoculation with the wild-type SARS-CoV-2 virus intranasally. Among those who participated, 17 of them had no infection at all. There was a single asymptomatic patient in whom, although no virus was detected in the participant’s throat, the researchers found antibodies in the bloodstream. The remaining 18 subjects were symptomatically infected. Both the virus and antibodies were present in their bloodstreams.
According to Dr. Yuhong Dong, Chief Scientific Officer of a Swiss biotech company and expert in antiviral drug development and infectious diseases, the natural immunity of the first 18 people was strong enough to win the battle against the virus without breaking a sweat. In comparison, the natural immunity of the latter half group was weaker. Their adaptive immunity had to intervene to fight off the virus, which resulted in the creation of antibodies, and the levels of inflammatory proteins in their bloodstream also increased. In the end, the infection was eradicated at the cost of sacrificing countless immune cells such as macrophages or natural killer cells.
So when being exposed to the same virus in the same way, why is it that some people don’t get infected and some do? To understand the mechanisms behind this, we first need to take a look at the human immune system.
5 Barriers of Human Immunity
Human immunity is similar to a multi-layered defense network and is composed of five barriers.
- Physical barrier
The first barrier of our immunity includes our skin, nose, and eyes. When viruses enter the body through breathing, the nose hairs will first try to block them, which become stimulated, resulting in sneezing. The nasal discharge and the mucus on the surface of the throat, trachea, and bronchus can trap the viruses, which are later expelled from the body by sneezing or coughing. The eyes work in a similar way by secreting tears to kill and remove viruses and toxins from the body.
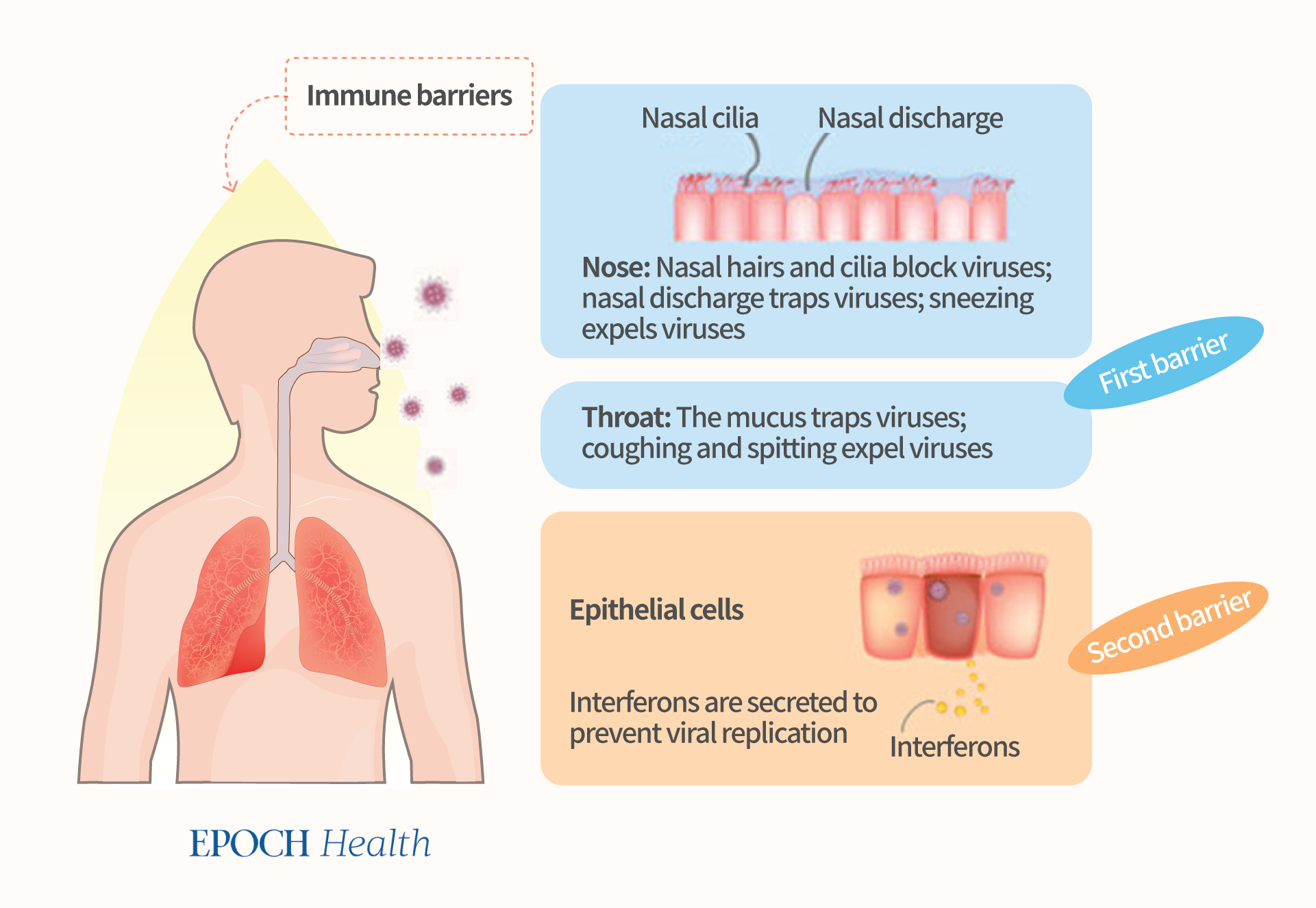
- Epithelial cell barrier and interferon
Epithelial cells are on the surface of our nose, throat, trachea, bronchi, and lungs; they make up the inner surfaces of our breathing organs.
When viruses invade epithelial cells, the latter automatically start their antiviral mechanism, mainly by producing interferons, which are important antiviral substances that can prevent the replication of viruses. In people with strong immunity, the mechanism of interferon secretion alone is sufficient to eliminate the viruses.
Interferons are produced by many immune cells (e.g. leukocytes, natural killer cells, natural killer T cells, and T cells). They don’t directly kill viruses. Instead, interferons “interfere” by instructing cells to produce many antiviral proteins and by enhancing the virus-killing mechanisms including intracellular pathways and activating innate immune cells.
The interferons produced in the early stage of a viral infection can delay the viruses’ replication and so delay their spreading to the entire body, thus buying time for the body to clear the viruses so that the chance of developing any illness is reduced.
Dr. Vincent Feuillet from the French National Institute of Health and Medical Research (INSERM) published an article in 2021 in the journal Trends in Immunology. According to the article, the outcome of a COVID-19 infection depends on an individual’s ability to produce type I interferons (IFNa/ß) rapidly. If the body has this ability in the early stages of the infection, the viruses can be eliminated directly and quickly, and there is little room for them to survive. On the contrary, if the body does not produce any interferon, or the body is in a state of chronic inflammation, one cannot quickly eliminate the viruses and the result is a harmful inflammatory response.
Therefore, the body’s rapid ability to produce interferons ensures the success of the battle with a virus, like the first and second groups of the UK challenge trial.
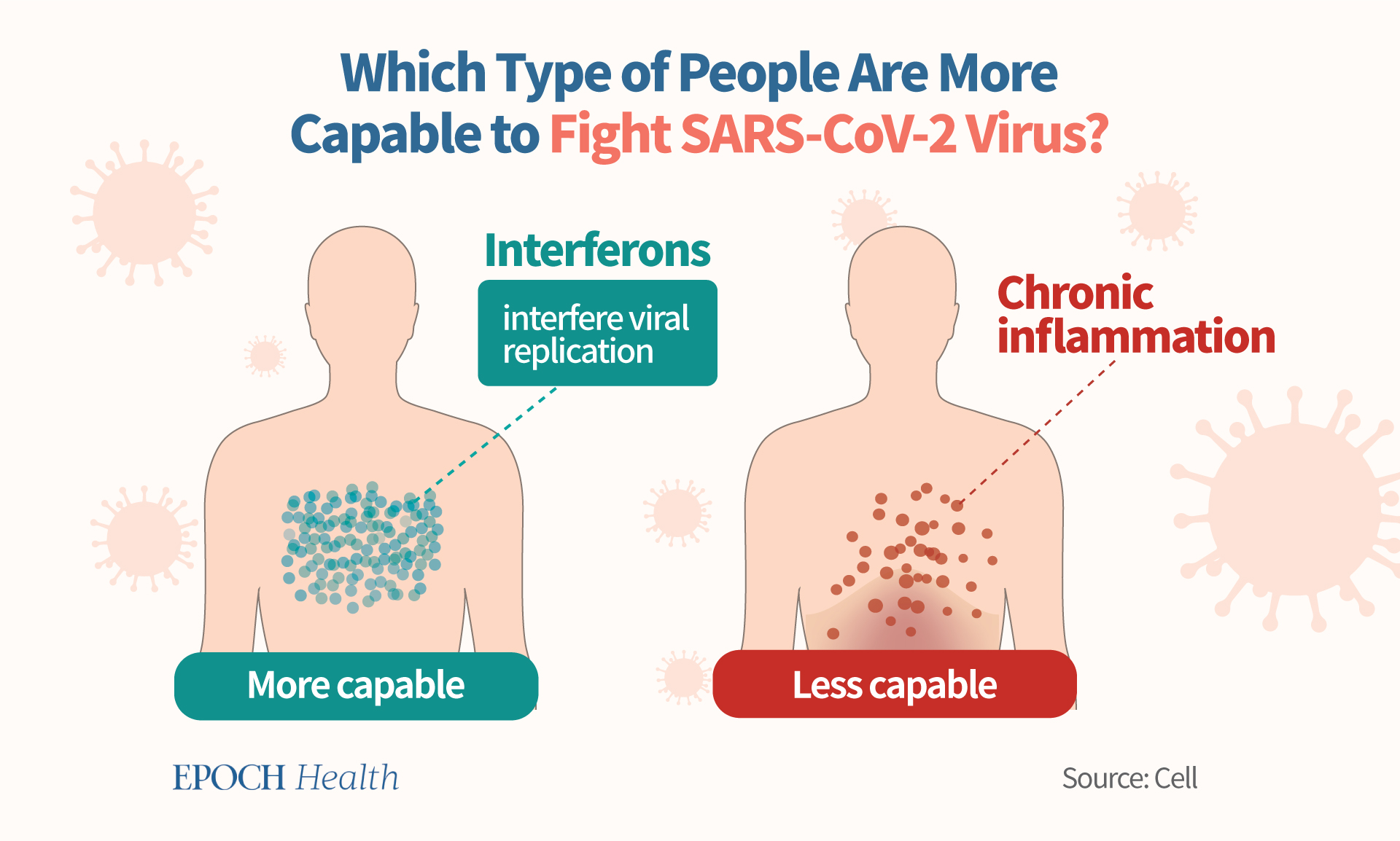
This study has shown the proven important role of interferon in COVID-19. People who secrete more interferons in the early stages of the COVID-19 infection will most likely have a mild disease. Researchers from the University of Louisville published an article in 2021 in the journal Nature, stating that there is a strong inverse correlation between the interferon response induced at the early stages of an infection and the severity of the disease. That is, the higher the interferon expression, the milder the disease will be.
- Innate immune cellular barrier
As the Omicron subvariants have greater transmissibility than the previous strains, scientists are concerned about the possibility of immune evasion and are actively developing new vaccines to deal with new variants. In fact, there’s no need to panic, as if the first three human immune barriers are strong enough, and they can resist all kinds of COVID-19 variants independent of gene codes and solve the problem of immune evasion.
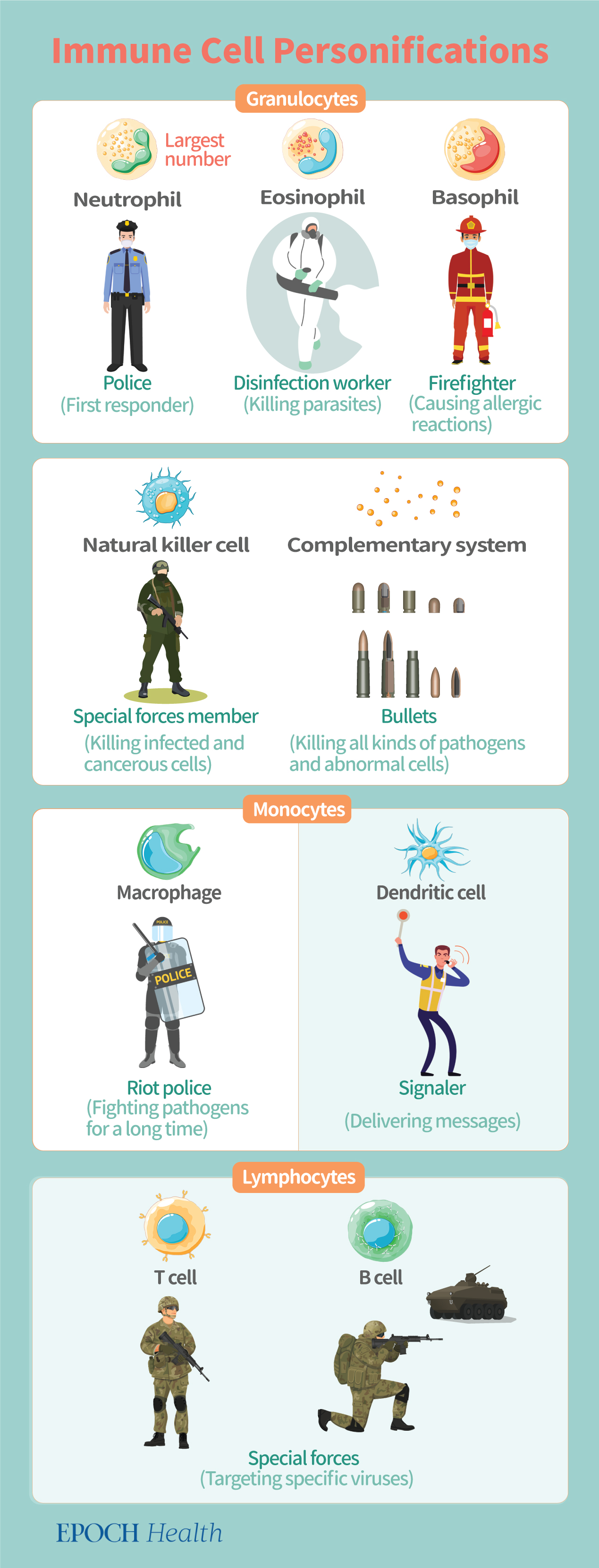
The third barrier is composed of innate immune cells, such as granulocytes, macrophages, dendritic cells, and natural killer cells.
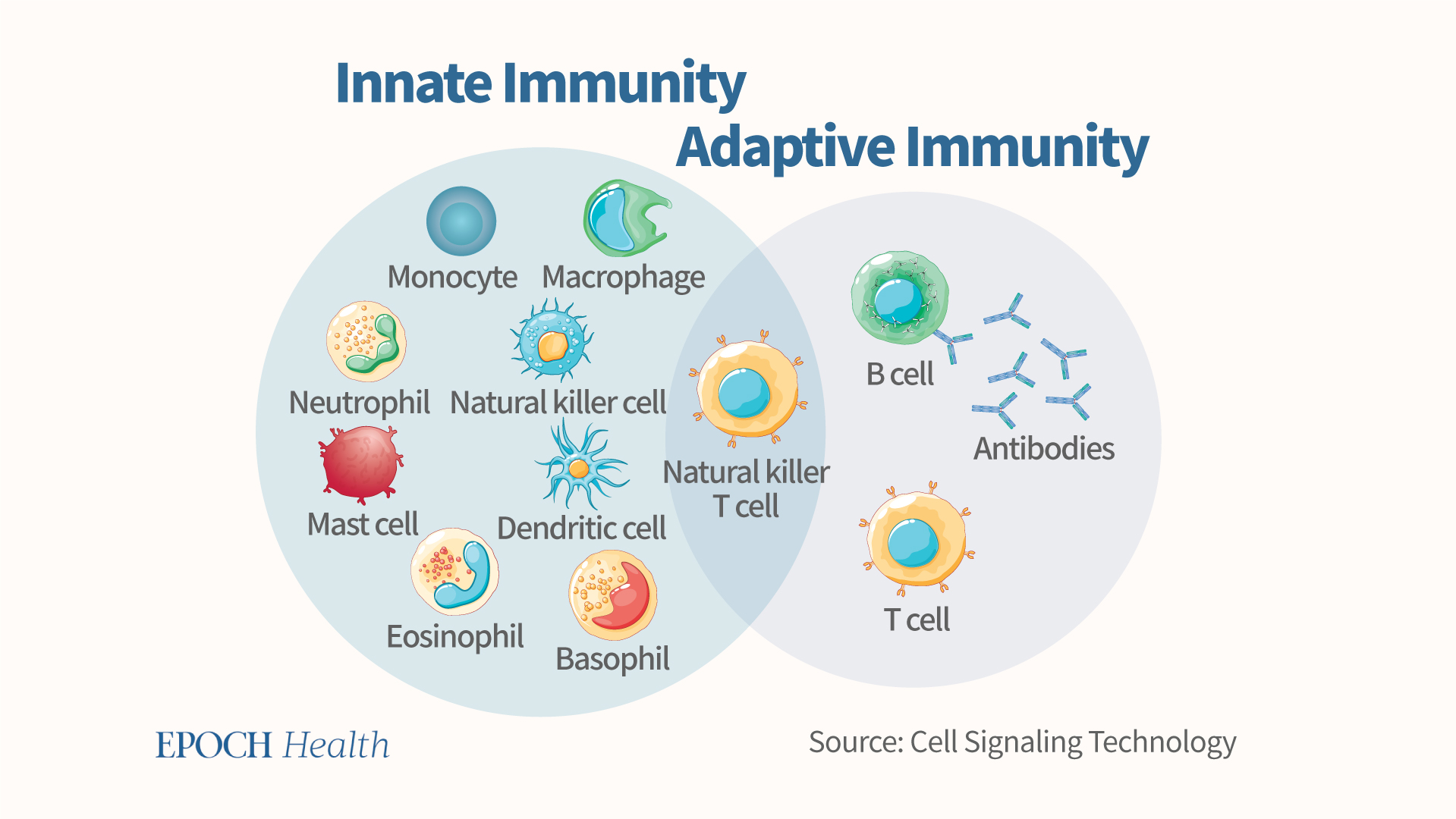
There are three types of granulocytes, including neutrophils, eosinophils, and basophils.
Neutrophils are the most numerous of the three in the body and are produced very quickly. They are the first responders to infections and play a police-like role in innate immunity.
Eosinophils are very effective in fighting against parasites. Parasites are multicellular organisms that immune cells have difficulty swallowing. However, rather than swallowing parasites, eosinophils attack them by releasing chemicals that penetrate their cell membranes, so eosinophils play the role of a “disinfection worker.” In addition, eosinophils trigger inflammatory reactions in the body by releasing chemicals. They are common factors in allergic reactions, like “firefighters.”
Macrophages can engulf pathogens in large numbers. In comparison with neutrophils, macrophages have a higher capability to attack pathogens and are able to fight them for a longer period of time. In addition to macrophages, there is also a type of dendritic cells that can swallow pathogens.
After macrophages and dendritic cells swallow a pathogen, they will analyze it and pass the relevant information to the acquired immune system for further action against the “enemies.” They are the “communication bridge” or “messenger” between the innate and acquired immune systems. Although their functions are similar, they have their own strengths. Macrophages are stronger in phagocytosis, like the “riot police”; while dendritic cells are better at analyzing and transmitting information, like “signalers.”
Natural killer cells are also part of the advance troops, the vanguard and frontline of the natural immune system, mainly responsible for killing virus-infected cells and mutated cancer cells in the body.
The complementary system is like bullets that can destroy various pathogens, bacteria, viruses or abnormal cells. In addition, it also promotes the ability of phagocytes to engulf pathogens through its “conditioning effect.” In other words, if pathogens were mashed potatoes then the complementary system would be the gravy that adds flavor to them, and encourages phagocytes to consume more pathogens. Furthermore, the complementary system can promote other immune responses, such as inflammatory responses and the secretion of immune-modulating substances.
- T cell barrier
T cells are lymphocytes, and they play a key role in the adaptive immune response.
Generally speaking, there are two major types of T cells, including the helper T cells and the cytotoxic T cells. The former “help” other cells of the immune system, while the latter kill virally infected cells and tumors. T-cells have many receptors on their surfaces, and they can only bind to one shape of antigen. When a T-cell receptor fits with its viral antigen on an infected cell, the cytotoxic cell will releases cytotoxins to kill that cell. Cytotoxic cells can also kill foreign and cancer cells.
T helper cells take a leading role in the fight against viruses and are like the “generals” of adaptive immunity.
- B cell barrier
The last immune barrier is composed of B cells, which are another type of lymphocytes. B cells create antibodies, which bind to pathogens or toxins to neutralize them. In addition, B cells can present antigens and secrete cytokines.
Compared with the first three lines of barriers, the reactions of T and B cells are relatively slow, and they are greatly affected by the specific viral genes and proteins. For instance, different COVID-19 variants require different T and B cells.
Therefore, it’s necessary to attack the cells directly infected by the virus according to the characteristics of the antigen.
If the B cells were mainly activated by vaccination, when a new variant emerges with a lot of mutations, the original antigens may not work, and new vaccines must be continuously developed to keep up with the viral mutations.
A Sensible Way Forward
If we are purely relying on the vaccine to fight against SARS-CoV-2, COVID-19 vaccines need to be continuously updated to keep up with the different strains’ constant mutations.
However the time to produce a new COVID vaccine is on average at least 8 months, which is far behind the speed at which the virus can mutate. A major new mutation has taken the stage every four or five months, as we have witnessed at least seven major strains (original strain, D614G, alpha, beta, delta, omicron BA1, BA4/5) during the past 32 months of the pandemic.
Luckily, people have the first four front layers of immunity, which could help us defend well against any virus, independent of the B cells or neutralizing antibodies.
According to Dr. Dong, a more sensible, rational, and effective way to avoid COVID-19 infection is to boost our natural innate and adaptive immunity so that it’s strong enough to protect us, just like the first two groups of subjects in the UK human experiment trial mentioned earlier.
We can do several things to improve our innate and acquired immunity. For instance, a diet rich in nutrition, a healthy work and rest schedule, and a stable and cheerful mood are all important. Furthermore, although it may sound inconceivable, honoring traditional values, as well as being more considerate for others can significantly improve the overall immunity of our cells.
Once we have a strong immunity, it’s possible for us to peacefully coexist with COVID-19 viruses without worrying about mutantations or expired vaccines.
Fuel Your Immune System
We need to pay attention to our intake of basic nutrients, and properly supplement vitamins and trace elements to maintain the normal structure and function of our first immune barrier.
Besides providing fuel and building blocks for the immune systems to function and produce proteins and new cells, diet provides the nutrients used in immune cell metabolism and antiviral functions.
Adequate micronutrient intake should include:
- Vitamin C: It can help with the differentiation and proliferation of T and B cells. A lack of vitamin C will lead to impaired immunity and higher susceptibility to infections.
- Vitamin D: It can reduce the incidence and severity of virus infection. A study has shown that adequate serum vitamin D level could protect us against severe COVID-19.
- Zinc: It helps activate white blood cells (i.e. immune cells) and is essential for wound healing. Zinc-rich foods in daily life include meat, spinach, and nuts.
Furthermore, vitamin C, vitamin E, zinc, selenium, and omega-3 fatty acids can protect the body from oxidative and inflammatory stress.
Things to avoid include:
- High intake of salt: It destroys beneficial gut bacteria, thus increasing chronic inflammation in the intestines, which is detrimental to the immune system’s antiviral efforts.
- High intake of sugar: It damages phagocytic cells (which swallow germs) and gut microbes. Consumption of sugar causes chronic inflammation, harms the interferon secretion in epithelial cells, and impedes the antiviral function of natural immune cells, T cells, and B cells.
Healthy Habits
In order to reduce the chance of COVID-19 infection, please pay attention to personal hygiene. For example, wash our hands and shower frequently, to remove the viruses if we have been exposed to them.
We can quit smoking, as it damages the structure of the skin, accelerates skin aging, and destroys the ability of respiratory epithelial cells to produce interferons. Furthermore, smoking has been found to be associated with more severe illness and an increased risk of death after hospitalization due to COVID-19 infection.
On a similar note, we can also avoid drinking alcohol, as it damages epithelial cells, T cells, and B cells.
Maintaining a healthy work and rest schedule, including getting quality and adequate sleep at night, is important for our immune system to self-recover and operate at its full capacity. During sleep, important hormones (growth hormone and melatonin) are released by the body, and melatonin enhances both innate and cellular immunity.
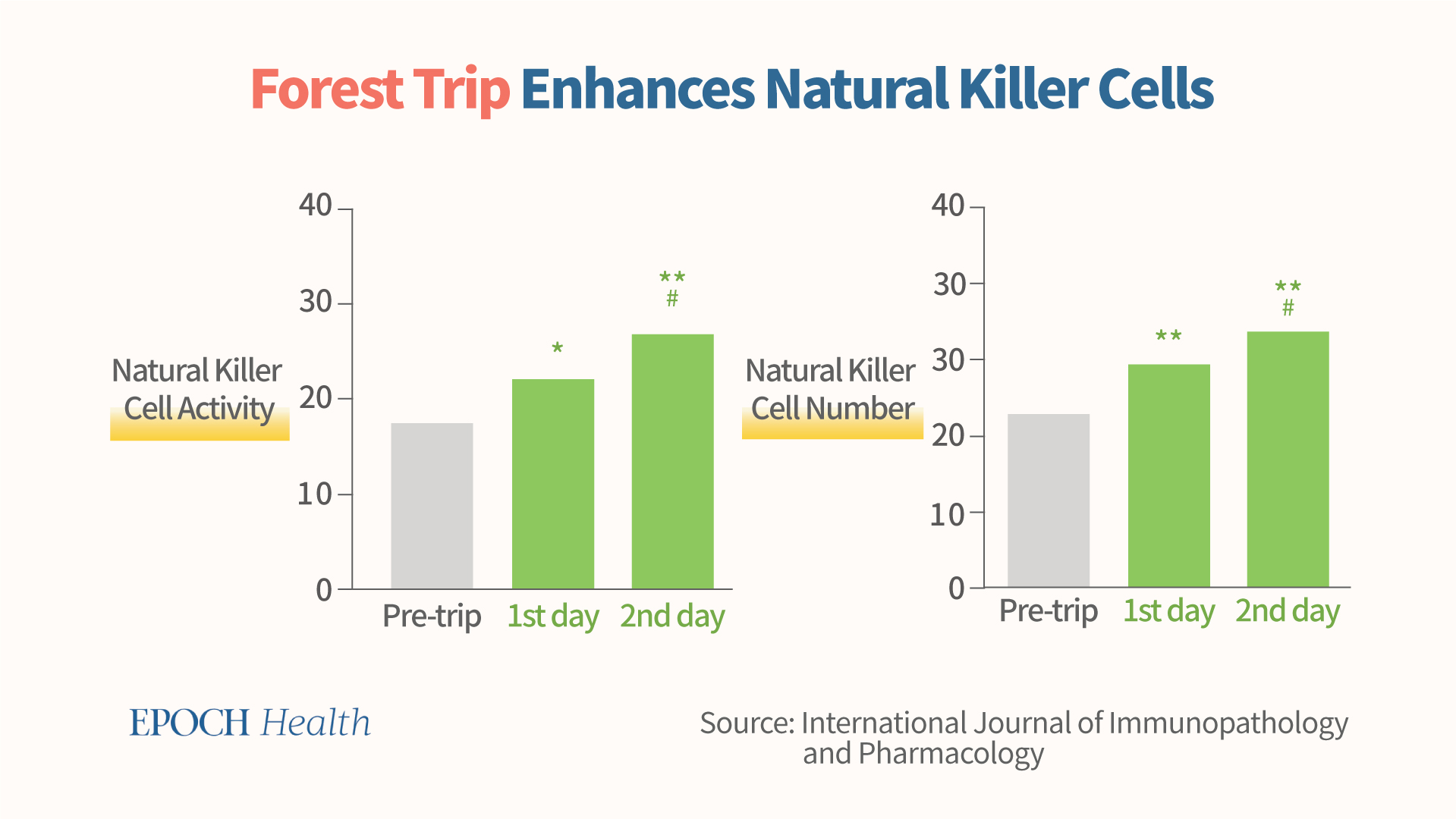
Make some time to exercise and be close to nature. For example, forest bathing trips can boost natural killer cell functions. These are short leisurely visits to a forest. A series of studies have discovered that such trips resulted in an increase in natural killer cell activity, as measured by increases in the number of natural killer cells and the elevated levels of certain cytolytic immune proteins.
Exercising can also help us maintain a healthy body weight, as obesity triggers a chronic inflammatory state and counteracts the immune system’s antiviral abilities.
We can also practice sitting in meditation to enhance our immunity, as meditation reduces chronic inflammation, maintains cell rejuvenation, and enhances antiviral ability. A large number of studies have suggested that meditation, Tai Chi, and qigong have positive impacts on the immune system, boosting our innate antiviral immunity and keeping us away from chronic inflammation.
Mental Health and the Spirit
In an article published in the journal Brain, Behavior, Immunity in February 2021, several scholars from the United Kingdom and Taiwan suggested that in addition to the current pharmacological treatments for COVID-19, psychological support should also be implemented to improve people’s mental health and enhance their psychoneurological immunity to the pandemic.
Due to the virus’s complexity and variability, traditional medication or allopathic treatment alone does not work well. We may consider tapping into the spiritual aspect, and use healthy lifestyle and psychological interventions to enhance our overall immunity and self-healing ability.
Inner Peace
According to a paper published in the journal Brain, Behavior, Immunity, depressed people have reduced lymphocyte responses, weakened T-cell immune responses to viruses, and reduced NK-cell activity, resulting in an overall trend of reduced antiviral immunity in the human body, making people vulnerable to viral and bacterial infections.
In addition, depression also increases the production of inflammatory substances, such as pro-inflammatory cytokines and chemokines, leading to a chronic inflammatory state. Furthermore, negative emotions combined with stress can reduce the body’s immunity, adding to the vicious cycle that makes people more susceptible to the COVID-19 infections.
To break the vicious cycle, we may have to put down those painful secular goals so as to achieve better inner peace. Letting things naturally unfold is sometimes a release, and maintaining a cheerful mental status helps nourish our immunity.
Here is an example. Typically, the immunity of the elderly is reduced. However, a 117-year-old French nun, Europe’s oldest person, notably recovered from a COVID-19 infection in early 2021. According to Dr. Dong, this woman’s recovery is probably due to her “kind and peaceful state of mind related to her belief.”
How can one achieve inner peace? Staying honest is another way.
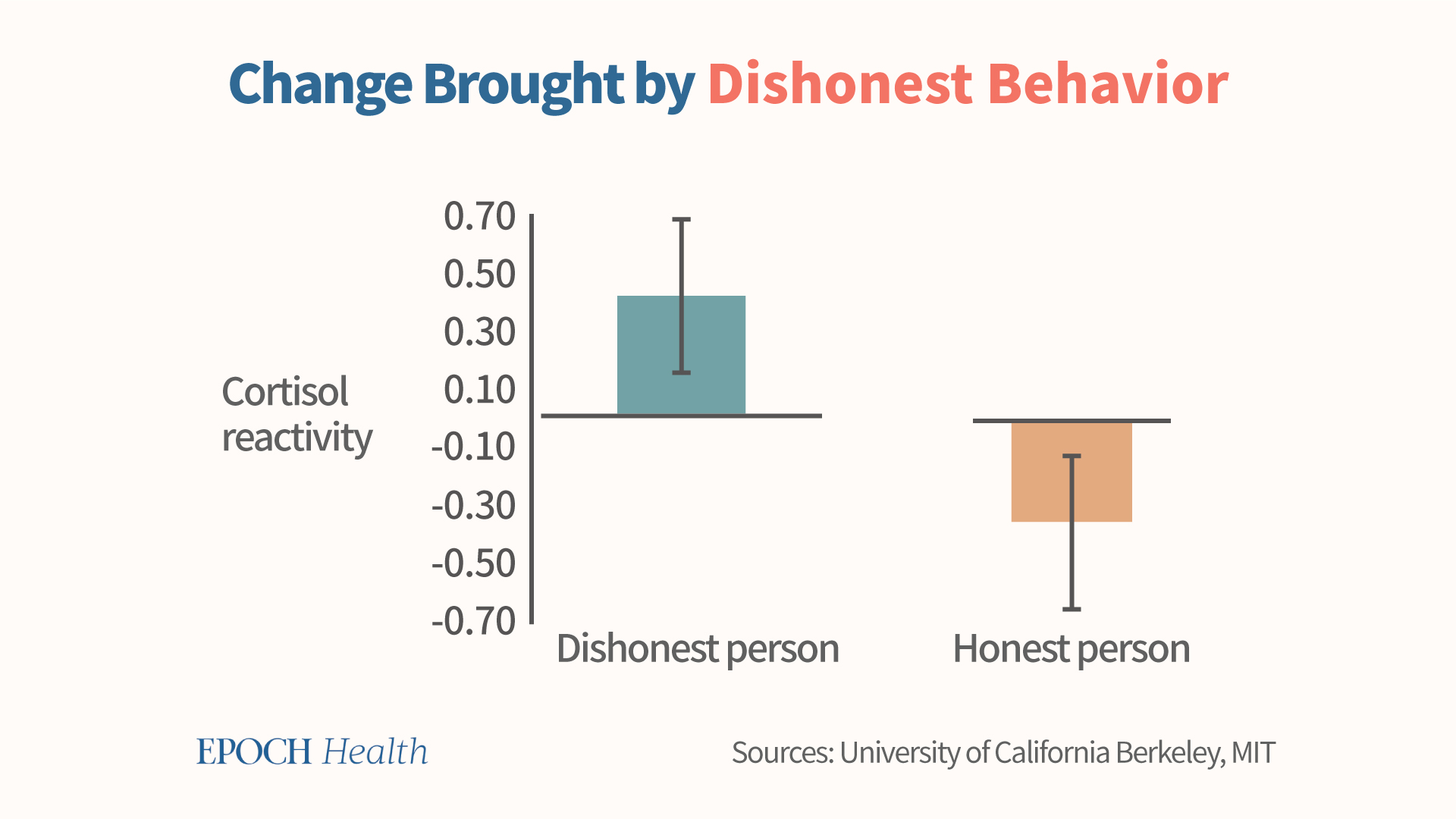
Dishonesty harms our immunity. When someone lies, his cortisol level is higher than normal. In fact, cortisol reactivity is significantly higher in people who lie than in truth tellers.
The higher the cortisol reactivity, the more likely that this stress hormone’s level is elevated in the body. Corticosteroids have a suppressive effect on immune cells, thus inhibiting the body’s ability to fight viruses. Therefore, in the midst of the pandemic, dishonest behavior can lead to a decrease in one’s own immunity.
Follow Traditional Values
Believe it or not, following traditional values can also improve the overall immunity of cells. An article published in 2021 in the journal Anxiety, Stress & Coping suggests that three strategies developed from evidence-based medical research can help people reduce anxiety, stress, and depression, and can help them get out of the pandemic faster.
These three strategies are following typical traditional values: fostering a sense of social belonging, practicing compassion, and engaging in kindness.
Compassion and Kindness
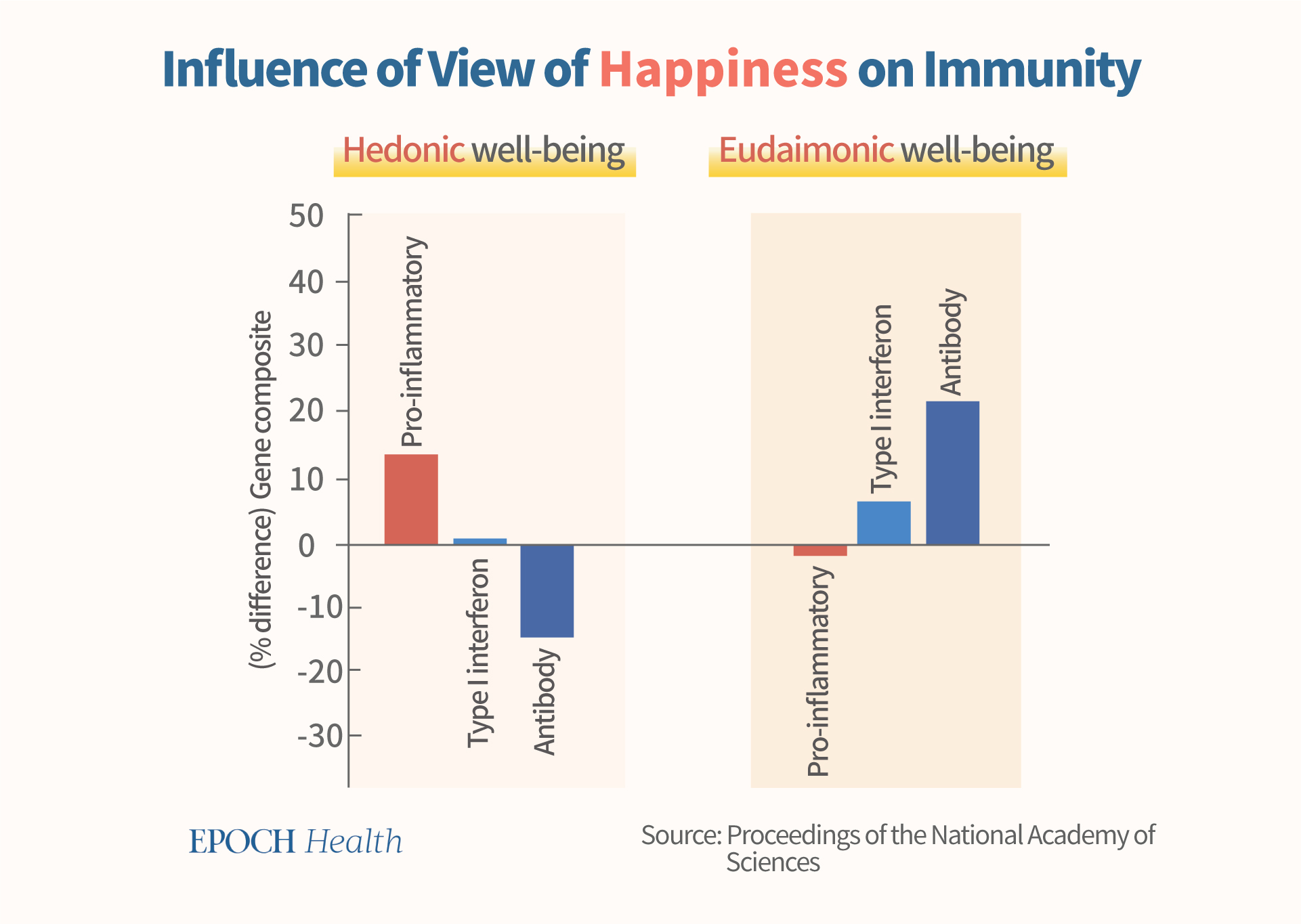
In a 2013 study published in the Proceedings of the National Academy of Sciences (PNAS), the immune system indicators of people with two different views of well-being were examined. One view is eudaimonic well-being, which is inclined to pursue human justice and noble goals, and hedonic well-being, which is more inclined to pursue personal sensory enjoyment. It was discovered that people of eudaimonic well-being have higher gene expression of interferons, higher antibody production ability, and significantly lower expression of inflammatory genes. The overall effect of their gene expression is more favorable for their body to fight against viruses, including SARS-CoV-2.
According to Dr. Dong, in the midst of the pandemic, there’s much more one can do to boost immunity than simply diet and lifestyle. It’s also of great benefit to advocate for the traditional values of honesty, kindness, and tolerance. Tapping into spirituality can also help enhance the body’s antiviral potential, and help people better cope with the lingering effects of the pandemic, and any other emerging viruses as well.
References
https://www.cell.com/action/showPdf?pii=S1471-4906%2820%2930261-1
Nutrition and immunity: lessons for COVID-19 | European Journal of Clinical Nutrition
Vitamin C and Immune Function – PMC
Mechanisms in Which Smoking Increases the Risk of COVID-19 Infection: A Narrative Review – PMC
Melatonin, immune function and aging – PMC
Effect of forest bathing trips on human immune function – PMC
The Effects of Tai Chi and Qigong on Immune Responses: A Systematic Review and Meta-Analysis – PMC
https://www.pnas.org/doi/epdf/10.1073/pnas.2110455118
The three frontlines against COVID-19: Brain, Behavior, and Immunity – PMC
Depressive disorders and immunity: 20 years of progress and discovery
Europe’s oldest person, 117-year-old French nun, survives COVID-19 | Reuters
https://haas.berkeley.edu/wp-content/uploads/Carney.HowPowerCorrupts.pdf
A functional genomic perspective on human well-being | PNAS
Views expressed in this article are the opinions of the author and do not necessarily reflect the views of The Epoch Times. Epoch Health welcomes professional discussion and friendly debate. To submit an opinion piece, please follow these guidelines and submit through our form here.

